In today’s PhysioRoom blog we’re going to dig deeper in to ligaments.
Not literally, of course, as that would be rather painful, but we are going to take a more in depth look at the process in which ligaments are injured and how exactly they repair.
If the bones are the bricks, the building blocks of the human body, then ligaments are the cement that holds them all together, that’s why it’s vitally important to look after them, as without them, your body would be a useless bag of jangling bones.
And what’s the first step in looking after anything? That’s right, the knowledge of what something actually is, so let’s get straight to it…
So what are ligaments?
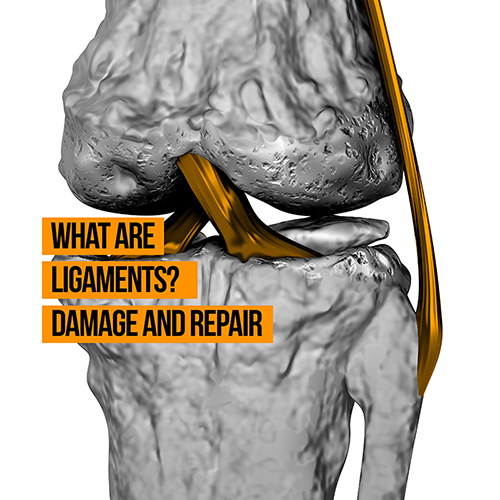
We already made the cement and bricks analogy, but to look at it a bit more literally, ligaments link bones to other bones and provide support to the joints.(Not to be confused with tendons, which connect muscle to bone)
Their length, strength and position determine the range of movement within a joint, not allowing the joint to move outside of this range where they become unstable. To be able to do this, ligaments must possess immense mechanical tensile strength.
Ligaments are classified as dense connective tissue, and they consist of a protein substance called collagen. The organisation of these collagen fibres give the ligament is tensile strength.
Another important function of ligaments is to provide proprioceptive input to the brain that allows a person to know what position the joints are in, without having to look or think about it. It’s this sense that helps us perform the complex coordinated activities needed for sport.
What is Collagen?
Collagen is a fibrous protein that makes up a third of the protein in the human body. The molecules in most collagens are packed together to form long thin fibrils, anchoring cells to each other.
Despite their being at least 16 different types of collagen, all with different types of structures and functions, but 80 to 90 percent of them in the human body belong to types 1, 2 and 3.
Collagens in the human body are tremendously strong and flexible, with type 1 collagen fibrils particularly capable of being stretched. In fact, gram-for-gram, they are stronger than steel.
A normal ligament consists of:
- 90% Type 1 collagen
- 9% Type 3 collagen
- 1% fibroblast cells (the cells that produce collagen)
Type 1 collagen is mature collagen tissue and has the greatest tensile strength, whereas type 3 collagen is immature collagen tissue and doesn’t provide a great deal of tensile strength.
After being laid down by the fibroblast cells, it takes around three months for type 3 collagen to mature in to type 1. Much like with other cells in the body, this process of renewal occurs continually.
When ligament tissue is examined under a microscope (see diagram) it can be clearly observed that the collagen fibres are arranged in a longitudinal pattern to resist the stress that is placed upon the ligament. This arrangement means a great deal of force is required to damage ligaments.

In a collision sport like football, this force is generated by opposition players or when a player catches his foot in the turf and his whole body-weight goes over one particular joint, like during a knee ligament injury.
This force produces structural damage to the joint capsule and the ligaments, which is more commonly known as a ligament sprain.
Ligament sprains are classified as follows:
GRADE 1 SPRAIN – There is damage to a few collagen fibres, producing a local inflammatory response. This is characterised by pain over the affected ligament.
GRADE 2 SPRAIN – There is damage to a more extensive number of collagen fibres. This produces a more marked inflammatory response characterised by intense pain and joint effusion (swelling).
GRADE 3 SPRAIN – The damage to collagen fibres is such that there is a complete rupture of the ligament. This produces intense pain, joint effusion and marked joint instability. Surgery may be necessary to restore joint stability.
Ligament Repair Process
As with other soft tissue injuries, ligament healing consists of a period of inflammation followed by repair and then remodelling.
Inflammatory Phase
The inflammatory phase follows trauma to the collagen fibres and depending on the severity of the injury, can last for 3-5 days. During this period, there is bleeding in the tissues and chemicals are released which produce pain.
This, together with fluid from the damaged cells, produces swelling within the joint, piling pressure on the nerve endings, thus causing more pain.
Rehab times can be greatly reduced by appropriate treatments in this acute stage. These appropriate treatments would usually consist of protecting from further damage (e.g. the use of crutches), rest from activity involving the injured body part, ice (never apply ice directly to the skin), compression, elevation and potentially the administration of some anti-inflammatory medication.
Repair Phase
The repair phase is mediated by blood clotting over the damaged tissue. Blood platelets form a mesh to initiate healing.
Also present in the blood clot are fibroblast cells, which proliferate and begin to lay down Type 3 (immature) collagen tissue, between 3-21 days after the injury.
The use of electrotherapy in this phase has been shown to encourage fibroblast activity that ultimately provides a structurally stronger ligament.
Remodelling Phase
The remodelling phase follows the repair phase and can last for up to a year, in which maturation of collagen tissue from Type 3 to Type 1 and realignment of collagen tissue takes place.
When it is first laid down, the collagen tissue is haphazard and does not possess a lot of tensile strength, much like bricks and cement analogy, it first has to ‘set’.
Going forward, the ligament gradually becomes stronger through being subjected to controlled strain in a functional pattern, which aligns the fibres in a longitudinal fashion. Physiotherapy, in the form of controlled exercises progressing to functional activity, aid this process of remodelling.
Because the remodelling phase lasts for up to a year, there is a potential weakness in the ligament and a risk of re-injury.
This risk is reduced by providing additional stability with strapping, increasing the strength of muscles which also provide support to the joint, and by doing proprioceptive exercises to increase the patient’s sense of joint positioning.