What is Osteoarthritis of the Knee?
Arthritis (osteoarthritis) is a common cause of knee pain and knee swelling that usually manifests itself in middle age. The term osteoarthritis is somewhat misleading, because it’s literal meaning is ‘joint inflammation’. Although there is a component of joint inflammation with this condition, the primary process of tissue damage is progressive knee joint degeneration. In order to fully understand arthritis of the knee, it is probably helpful to review the anatomy of the knee joint.
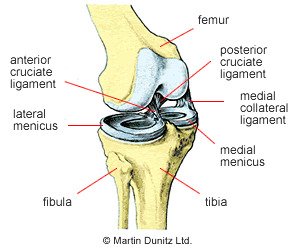
The knee is a ‘synovial joint’, which means it is enclosed by a synovial capsule that contains synovial fluid. The joint surfaces of the femur (thigh bone) and tibia (shin bone) are covered by ‘hyaline cartilage’, which provide friction free movement (coloured light blue in the diagram). The semi-circular structures sitting on top of the shin bone are the two menisci. The menisci are shock absorbers that are made of ‘fibrocartilage’ and are commonly called cartilage. As can be seen, the knee joint has a medial (inside) and lateral (outside) ‘compartment’ and one or both of these can be affected by arthritis.
Damage to the ‘articular’ or hyaline cartilage can be as a result of sporting trauma, but is more commonly due to repetitive stresses over a long period of time. This is usually associated with habitual overuse of a joint for occupational or sporting purposes. In most individuals, the signs and symptoms may not appear until middle age, but the disease process starts much earlier and the arthritis process can be accelerated if the menisci or parts of the menisci have been removed previously. Removal of the menisci exposes the hyaline cartilage to damage.
The Hyaline cartilage is normally ultra smooth to allow friction free movement, but early damage to the superficial layers produces a frayed appearance. In time, with more stress, this frayed surface evolves into cracks or ‘fissures’ in the articular cartilage, which can leave the underlying bone exposed, causing pain.
With continued wear the underlying bone takes on a polished appearance and eventually micro-fractures appear. The body’s natural reaction is to attempt to heal the micro-fractures by laying down more bone. This leads to a thickening of the underlying layer of bone, which can be seen on x-ray. Another common feature on x-ray is the formation of bone cysts in the layer of bone beneath the joint surface, together with a flattening of the articular surfaces as the body attempts to spread the surface area over which forces are transmitted.
As well as changes in the articular cartilage and underlying bone, osteoarthritis produces soft tissue changes. As the joint becomes deformed by bony changes the ligaments which support the joint become stretched. There is also thickening and distension of the capsule that surrounds the joint and both of these features get progressively worse.
Knee Arthritis Signs & Symptoms
Although osteoarthritis is a progressive disease, the signs and symptoms of the condition rarely get worse in a linear fashion. Often people in their thirties or forties will ‘over do it’ one weekend, either in sport or in the garden, and they will experience a flare up from the degenerate joint. This flare up may last for 48 hours and usually consists of stiffness (particularly in the morning), pain and swelling of the affected joint. The knee may, but not always, make a creaking or grating sound as the process progresses.
A substantial time period may pass before there is another flare up, but each flare up will get progressively more intense. Also, as time goes by and more stress is put on the affected joint, the time interval between flare ups will decrease to the point where, eventually, the person will have pain even at rest.
As the disease progresses the symptoms that start off being triggered by over activity, become triggered by immobility. Whereas, in the early stages, rest is essential during a flare up period, disuse in the later stages will exacerbate the problem. This is because the dynamic stability provided by the muscles surrounding the joint is lost if there is muscle wasting due to inactivity. This puts even more strain on the ligaments and ultimately the joint surfaces themselves – producing more pain. In the later stages, if there is pain at rest and during the night, as well as problems with mobility, then joint replacement surgery is appropriate.
What you can do
- Consult a sports injury expert
- Apply ice packs/cold therapy
- Wear a knee brace for support & reassurance
- Wear supportive insoles to control pronation
- Use a buoyancy aid for pool exercises
Knee Arthritis Treatment
Patient education is one of the most effective treatment strategies. By understanding the nature of osteoarthritis the patient can make adjustments to their lifestyle that will make the problem more manageable. In summary, the patient must understand that too much activity or too little activity will make the problem worse. Each individual is different but, over time and through experience, each person will learn the optimum level of activity for their affected joint.
During the early phase flare ups are best treated symptomatically. NSAIDs prescribed by a doctor are effective in relieving pain and inflammation. An ice pack may be used to relieve a hot painful knee joint. Ice packs can be applied for periods of twenty minutes every couple of hours (never apply ice directly to the skin as it can cause an ice burn). The ice packs relieve pain and reduce bleeding within the tissue. A cryotherapy cuff is the most effective method of providing ice therapy and can be used for the home treatment of knee injuries and knee pain. It can provide continuous ice cold water and compression for 6 hours, significantly reducing knee pain and knee swelling.
Many people find that wearing a arthritis knee brace can help provide support and reassurance. As arthritis of the knee tends to be more painful during cold winter months, a neoprene support is often helpful as it provides soothing warmth to the joint.
Once arthritis of the knee has been formally diagnosed a more long term preventative strategy can be undertaken. This is aimed at reducing pain and stiffness and maintaining range of movement in the affected joint. A sensible approach can prevent excessive degeneration which may eventually lead to disability.
Each individual case is different and a full assessment by a chartered physiotherapist will identify factors that may exacerbate the problem. Once identified, the physiotherapist will formulate a strategy to address these problems and provide advice on how to make changes and adapt your lifestyle to allow as normal activity as possible. It may be that a work task is putting excessive repetitive stress on the affected joint. It may be possible to modify the task so it can be done in a different position, or specially adapted equipment can be used to reduce the repetitive loads. The main problem may be due to posture or a malalignment of the body. If so, this can be remedied through corrective exercise, orthotics (insoles) or a knee brace.
Where the knee joint is affected maintenance of full range of motion is encouraged to reduce stiffness. Knee bend can be lost if the person doesn’t use the full range of motion because of pain. Pendular exercises (gently swinging the foot back and forward) to encourage knee movement may be helpful. A physiotherapist can use manual techniques to help maintain the range of movement.
Keeping the neighbouring joints strong will also help to dissipate the load if the lower limb is affected. If the pain is felt at the knee, a strong healthy ankle and hip joint will both help reduce the work needed at the knee. Using equipment like a wobble board to maintain good balance and proprioception will ease the demand on the knee joint.
Pain in the knee joint can lead to wasting and weakness of the quadriceps (thigh) muscles. This leads to a vicious circle of further joint instability and more pain, leading to more inhibition and muscle weakness. Exercises to maintain quadriceps and hamstring muscle strength are encouraged to provide support for the affected joint. This strengthening should be done under the supervision of a physio. If there is pain during or following the exercises then the weight used is probably too high.
If the knee joint is affected then weight bearing activities can make the problem worse. Running on a hard surface increases the stress on the articular surfaces and is not helpful for a person with osteoarthritis. Cycling and swimming, because of their partial weight bearing status, are much more beneficial for the person with osteoarthritis of the knee (note: breaststroke should be avoided, particularly in those with osteoarthritis of the medial compartment of the knee).
During this time, knee function can be enhanced by performing non weight bearing exercises in the pool. The use of a buoyancy belt allows an early return to swimming pool exercises for people with arthritis of the knee. It clips around the waist and allows the user to run without putting weight through their injury.
Knee Arthritis Prevention
In addition to avoiding weight bearing and impact exercises, kneeling should be avoided, as should sitting in one position for a period of time. Frequent breaks should be taken to stretch and take the knee joint through it’s full range of motion, as the articular cartilage draws most of it’s nourishment from the synovial fluid within the joint, and this has the effect of providing nutrients to the joint surfaces.


