The medial collateral ligament is the primary stabiliser of the inner (medial) side of the knee. It is a thick fibrous band and is designed to resist valgus (side-on) forces to the knee.
The onset of a MCL sprain is usually traumatic and can happen via a direct blow to the outside of the thigh. Or the MCL can be torn when the foot is planted and there is a valgus strain put on the knee. It can be aggravated by walking on uneven ground or changing direction sharply when running.
This often happens in football tackling injuries. Occasionally this injury can happen when there is a valgus stress placed upon the knee in conjunction with the femur externally rotating. This type of injury often occurs while skiing.
Pain, swelling and instability are all common with this injury. It is possible that you will lose some joint range of motion and struggle to weight bear initially, if it is a substantial injury.
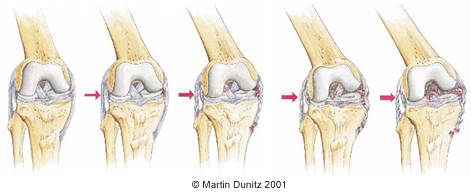
Tears to the MCL are classified as follows:
Grade 1: Tearing of a few fibres but no ligament laxity or joint instability is present.
Grade 2: Tearing of a substantial amount of fibres, with mild ligament laxity and joint instability present.
Grade 3: A complete tear of the mcl fibres, ligament laxity and joint instability are both present
MCL Sprain Rehabilitation
Here we present an example of a rehabilitation programme for a professional footballer with a grade II medial collateral knee ligament sprain.
Acute Phase (Days 1 to 3)
- Rest from activity.
- Protect the injury site from further damage by using crutches to avoid putting any weight through the injured leg.
- Apply ice packs or a cryotherapy device for 20 minutes every 2 hours (never apply ice directly to the skin). This will have pain-relieving effect and also help to control the swelling.
- Apply a compression bandage to limit the joint swelling. The injured knee should be elevated in order to control and reduce swelling.
- Oral anti-inflammatory medication may be prescribed by a doctor.
Sub-acute Phase (Days 4 to 14)
- Continue to rest the injured part completely.
- Continue to protect the injured knee from further damage by using crutches. If it is not too painful it may be possible to begin partial weight-bearing on the affected leg whilst continuing to use the crutches.
- To further protect the knee a hinged knee brace should be used to prevent stress on the medial ligament. This should be locked between minus 10 degrees of extension and 90 degrees of flexion.
- Once the inflammatory response from the damaged tissue has settled (after 3-5 days) the ligament begins to lay down scar tissue to repair itself. It is thought that this process can be encouraged with the use of electrotherapy treatments such as ultrasound and pulsed short-wave diathermy.
- Begin ankle and hip range-of-movement exercises.
Early Active Rehabilitation Phase (Weeks 2 to 4)
- The hinged knee brace should be worn at all times during the early active rehabilitation phase, and should be set between minus 5 degrees of extension and 110 degrees of flexion.
- Provided it is not too painful, full weight-bearing should be encouraged and the crutches should be abandoned.
- A normal gait pattern should be present, with the heel striking the ground first and the toes pushing off for the next step.
- Isometric quadriceps should be performed in the pain-free range of movement. Straight leg raising should be performed to reinforce quads contractions.
- Gentle range-of-movement exercises should be encouraged between 90 to 30 degrees of knee flexion.
- Early proprioception exercises should be initiated.
Active Rehabilitation Phase (Weeks 4 to 6)
- The hinged knee brace should be worn at all times during the active rehabilitation phase. There should be no restriction of knee extension or flexion.
- Range-of-movement exercises should be continued.
- When range of movement allows, static cycling should be initiated.
- Isotonic muscle strengthening exercises should be initiated and resistance gradually increased (leg press/squats/ham curls/quads extensions).
- Continue proprioceptive training.
Late Active Rehabilitation Phase (Weeks 6 to 10)
- The hinged knee brace should continue to be worn, without restriction of knee extension or flexion.
- Range-of-movement exercises should be continued, until full range of extension and flexion is pain free.
- Isotonic muscle strengthening should continue, so that the affected knee’s quads and hamstrings have 90% strength of the unaffected knee.
- Continue static cycling and increase resistance.
- Initiate straight line running, gradually increasing the pace. Initiate ‘figure-of-eight’ running, gradually increasing turns.
- Begin ‘fitter’ exercises.
Functional Rehabilitation Phase (Weeks 10+)
- The hinged knee brace should be discarded.
- Isotonic muscle strengthening should continue.
- Continue to progress static cycling.
- Increase speed of running and increase turning angle to 180 degrees.
- Begin cliniband lateral agility/running exercises and star jumps. Hop distance should be 100% of opposite knee. Kicking the ball/block tackling.
References:
Marchant, Milford H et al. (n.d.) Management of Medial-Sided Knee Injuries, Part 1: Medial Collateral Ligament. The American Journal of Sports Medicine. [Online] 39 (5), 11021113.
Hanley, Jessica M. et al. (n.d.) Patient-Reported Outcomes After Multiligament Knee Injury. Orthopaedic Journal of Sports Medicine. [Online] 5 (3), 2325967117694818.


