What is a PCL Tear?
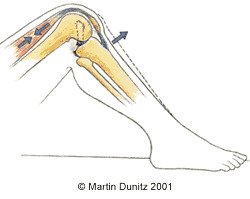
Posterior cruciate ligament (PCL) is located deep within the knee joint and PCL injuries are quite common knee injuries in sport. The PCL is larger and stronger than the anterior cruciate ligament (ACL). It passes backwards and downwards from the bottom of the thigh bone to the top of the shin bone. Its main purpose is to prevent the shin bone slipping backwards on the thigh bone.
PCL injuries are usually caused by a blow to the front of the upper shin. In motor vehicle accidents, this occurs as the top of the shin strikes the dashboard. In sports, a PCL injury can occur when an athlete falls to the ground on a bent knee, causing the upper shin to strike the ground first. A prominent tibial tuberosity (lump just below the knee cap) resulting from previous Osgood Schlatter’s disease may enhance the impact when the tibia strikes the ground.
One study estimates that PCL injuries make up as many as 20% of all knee ligament injuries, but the diagnosis is often missed. This is due to the fact that many people can function normally without a PCL. However, detection of PCL injury is important because untreated PCL ruptures will lead to significantly reduced stability and degeneration (i.e. osteoarthritis) of the knee and disability in later life.
PCL Tear Signs & Symptoms
Unlike those with ACL injuries, patients who have PCL injuries do not usually experience much knee pain or swelling. They usually report vague symptoms such as unsteadiness or insecurity of the knee. There may be pain or stiffness behind the knee with everyday activities such as getting up from prolonged sitting or kicking your shoes off with the affected side. Patients who have long standing PCL injuries that have never been diagnosed may report pain around the kneecap.
There are a number of physical tests that can be used to detect a PCL injury. One of the most widely recognised is the posterior drawer test. The test is done with the patient lying on their back, the knee bent to a right-angle, and the foot flat on the table. In this position, the Tibial Plateau should lie 1 cm in front of the Femoral Condyles. The degree of PCL injury is determined by the extent that the tibia can be pushed backwards by the examiner:
No Injury
The Tibial Plateau remains 1 cm in front of the Femoral Condyles.
Grade 1 Injury
The Tibial Plateau moves backwards but stays in front of the Femoral Condyles.
Grade 2 Injury
The Tibial Plateau moves backwards to lie level with the Femoral Condyles.
Grade 3 Injury
The Tibial Plateau moves backwards to lie behind the Femoral Condyles.
X-rays are useful to rule out avulsion fractures (where the PCL has been pulled away from one of its bony attachments). An MRI Scan is useful in confirming the diagnosis. However, when the injury is longstanding, an MRI may show an apparently normal PCL even though laxity may be present.

PCL Tear Treatment
Recommendations for treating PCL injuries vary greatly. However, sensible recommendations are as follows:
Patients who have grade 1 or 2 PCL injuries should first receive non-operative treatment that includes aggressive quadriceps strengthening and full range-of-movement maintenance alongside balance and stability exercises. Patients may return to sports when quadriceps and hamstring strength reaches 90% of the opposite side. This may take as long as 4-6 weeks.
The patient should follow this up every 2 years with x-rays and a bone scan, to monitor joint status. If early signs of degenerative joint disease appear on the bone scan, PCL reconstruction should be considered. Surgical treatment should also be considered if symptoms develop or if function declines.
Patients who have grade 3 injuries should be treated with PCL reconstruction. Before surgery the patient should undertake rehabilitation to regain full range of motion and quadriceps strength.
Patients who have avulsion fractures (where the PCL has been pulled away from one of its bony attachments) should be treated surgically.
Patients with PCL injury combined with significant ligament injuries should be treated with PCL reconstruction and repair of other injured structures.
What you can do
- Consult a sports injury expert
- Apply ice packs/cold therapy
- Wear a knee brace for protection
Following surgery, rehabilitation with a chartered physiotherapist is very important. The initial goals of physiotherapy treatment are to reduce knee pain and knee swelling. Ice packs can be applied for periods of twenty minutes every couple of hours (never apply ice directly to the skin as it can cause an ice burn). The ice packs relieve pain and reduce bleeding within the tissue. A cryotherapy knee cuff is the most effective method of providing ice therapy and can be used for the home treatment of knee injuries and knee pain. It can provide continuous ice cold water and compression for 6 hours, and significantly reduce knee pain and knee swelling.
Conventionally, following PCL reconstruction the knee is immobilised for a month, but now some pioneering surgeons are beginning knee range of motion exercise one week after surgery to prevent the excessive loss of critical range of movement that immobility can cause. Recent research has shown that it is safe to move the knee in closed-chain exercises (where the foot is in contact with a firm surface), although this should not be done without permission from the surgeon. Generally, regardless of surgical technique, patients remain in a knee brace and on crutches for 6 weeks.
PCL Tear Prevention
Proprioception training using a wobble board can help to reduce the risk of sustaining a knee ligament injury by strengthening the knee in all panes of movement. Also sport should be avoided if you are in a fatigued state as this can increase the risk of injury.


