What is a Osteitis Pubis Injury?
Osteitis pubis is a painful overuse injury that affects the pelvis and most commonly occurs during kicking activities, ice skating and dance. Running over rough, uneven terrain or slippery surfaces can also lead to the painful condition. It was first described by Legueue and Rochet in 1923. It affects an area at the front of the pelvis known as the ‘pubic symphysis’. The pubic symphysis is a cartilaginous (made from fibrocartilage) joint, that is tightly bound by very strong ligaments. This means that only a very limited amount of movement takes place at this joint.
Anatomy of Osteitis Pubis Injury
The exact mechanism of the development of osteitis pubis remains unclear. Several theories have been proposed, including the overuse of the abdominal muscles that attach to the pelvis causing gradual micro trauma to the bone; excessive shearing forces on the pubic symphysis caused by powerful kicking or repeated movements; or even instability of the saco joint at the back of the pelvis resulting in abnormalities, or malalignment at the pubic symphysis.
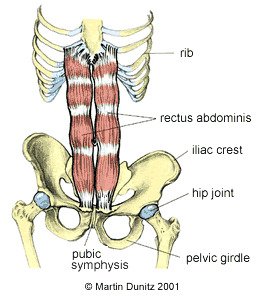
Osteitis pubis is most common in sports where a large shearing force goes across the pubic symphysis. This occurs during kicking activities, ice skating and dance. The excessive forces overstrain the pubic symphysis and cause an inflammatory response. This may involve erosion of the joint margins and is followed by a slow healing process. Others who tend to have a high risk of developing osteitis pubis include those with rheumatological diseases and expectant mothers.
Osteitis Pubis Signs & Symptoms
Osteitis pubis causes pain during and after exertion, which is often combined with tenderness to touch at the pubic symphysis area. Typically, this pain may radiate up to the lower abdomen or down to the groin region. In many cases the patient is unable to localise the pain, which may move around the pelvic region.
It is therefore important that all cases of persistent groin pain are referred to a doctor who can carry out a full assessment and make a differential diagnosis by excluding other conditions that may be potentially more serious.
The clinical signs and history of the patient are usually sufficient to raise the suspicion of osteitis pubis, but diagnostic investigations can confirm this condition. Plain x-rays can be useful. The patient may be asked to stand on one leg for these so called ‘stork views’.
The x-rays are able to see widening or erosion at the pubic symphysis which is indicative of osteitis pubis. An MRI scan may also be helpful as they clearly depict bone stress reactions and inflammatory changes in the tendons that attach to the pelvis. However, in the case of athletes and those who undertake a high level of sporting activity MRI findings may show bruising of the Pubic bone even in those who have no symptoms.
Osteitis Pubis Treatment
Frustratingly, osteitis pubis can be resistant to treatment and can last between 6 months and two years before symptoms resolve. It is a notoriously difficult condition to treat due to the location of the cartilage and minimal influence physiotherapy intervention can have. For this reason a preventative approach is preferable. Over training should be avoided, particularly in those who participate in long or repetitive kicking sports. Strengthening of the core muscles around the pelvic region is the most effective remedy as strong gluteal and abdominal muscles will help provide a natural ‘corset’ around the area and provide improved protection against injuries in this region.
Treatment options for those with acute symptoms are pretty limited. Rest is the most sensible approach – avoiding large scale movements, overstretching and uneven or slippery terrain, allows the affected tissue to settle down and heal (some MRI’s show the stress lines of micro fractures in the pubic bone, to give some idea of the degree of tissue damage). Non steroidal anti inflammatory drugs (NSAIDs) are advocated by some but this may not help the healing process if the damage is to the bone. In cases where bony damage is prevalent intravenous Biphosphates (or Bisphosphonates) may be a useful treatment. This drug is usually prescribed by a rheumatology consultant with the aim of treating osteoporosis (brittle bones). Biphosphates bind permanently to the surfaces of the bones and slow down the osteoclasts (bone-eroding cells). This allows the osteoblasts (bone-building cells) to work more effectively. Following this injection there is usually an improvement in symptoms within a month, although sometimes further injections may be necessary. Some people find that warm pants provide reassurance when returning to sports.
If the pain does not resolve with prolonged rest (and often it doesn’t) then corticosteroid injections may be considered. If the injection is successful the patient can usually return to activity within two to three weeks, although some people require a second injection. Some authors have reported good results using progressive stretching of the muscles that attach to the pelvis, but we find this is best done once the pain has settled. Improving hip range of movement is particularly important. Physiotherapy can help reduce tension in muscle groups such as the adductors, which may be overworking due to weaknesses elsewhere. Diagnosing these muscle imbalances is not a quick fix as it requires dedication to a stretching and strengthening regime. However, addressing such factors will lead to a better long term prognosis and reduced risk of the injury reoccurring.
In cases where osteitis pubis does not respond to conservative treatment within 12 months, some surgeons advocate a surgical approach. This is particularly the case if there is mechanical instability at the pubic symphysis. The surgeon uses a plate and screws across the joint to restore stability. Crutches are required for around 3 weeks and a return to sports is not possible before three months. The mechanism of surgical treatment is poorly understood. It could be that the restoration of stability reduces abnormal stresses, alternatively pain may be resolved by cutting through local nerve tissue. Of course it could be that the extended rest period is helpful.
Osteitis Pubis Prevention
Over training should be avoided, particularly by those who participate in long or repetitive kicking sports. Core strength and stability exercises are vital to improve muscle function across the trunk and pelvis. Core strength exercises on a mat using a swiss ball and resistance bands are ideal, because the improved muscular strength and stability can help to counteract the large forces that are applied to the lower abdomen and pelvis. This can reduce the risk of developing osteitis pubis. Seeking physiotherapy assessment for imbalances around the pelvic and groin muscles will also greatly help in the prevention of this painful condition.


