Achilles Tendinopathy
Achilles tendinopathy is the term used to describe all of the possible issues with an Achilles tendon including inflammation (tendinitis) or degeneration (tendinopathy). It is now believed that the Achilles tendon is not simply inflamed; instead, the tendon has become thickened and stiffens up.
Although this might sound alarming, degeneration (wear and tear) is largely rectifiable. Achilles tendinopathy can occur at the mid tendon or where the tendon inserts into the heel. If your pain is at the heel, insertion stretching the tendon and eccentric exercises should be avoided.
It is usually caused by training load error, in other words doing too much, too soon. It often occurs in runners who start doing more endurance, hills or speed sessions without adequate rest to allow the tendon to repair and become stronger. It may also happen in sports where there is a lot of sprinting or jumping.
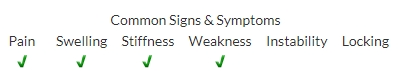
Symptoms:
Symptoms may occur at the start during or after the aggravating activity and include pain/tenderness/stiffness/swelling/clicking of the Achilles tendon. Pain when the tendon is compressed, discomfort when running or walking, especially on an incline/ decline.
Management:
It is worth seeing a physiotherapist to discuss the management of your Achilles tendinopathy. Often in acute (less than 6 weeks since onset) cases a modification of activity with a gradual re-introduction will be sufficient to reduce symptoms. There is strong evidence for the use of heavy slow resistance training, eccentric training and concentric training of the calf muscles. There is as yet no strong consensus over which method is the most beneficial and most research promotes a combination of these exercises. In more chronic cases, calf muscles and Achilles tendon strengthening and loading programmes will be required. This will include rest days between runs and not increasing tendon load by more than 10% per week. There is very limited evidence but some patients report that a heel raise reduces symptoms. Generally, symptoms improve after 12 weeks of rehab. If the episode continues for 6 months then surgery to remove adhesions may be offered. The use of ice is recommended to reduce pain and some may find that offloading the Achilles tendon by using k-tape is helpful.
References:
Wilson, F., Walshe, M., O’dwyer, T., Bennett, K., Mockler, D., & Bleakley, C. (2018). Exercise, orthoses and splinting for treating Achilles tendinopathy: a systematic review with meta-analysis. British Journal of Sports Medicine, 52(24), 1564–1574. https://doi.org/10.1136/bjsports-2017-098913
Malliaras, P., Barton, C., Reeves, N., & Langberg, H. (2013). Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Medicine (Auckland, N.Z.), 43(4), 267–286. https://doi.org/10.1007/s40279-013-0019-z

